National Insurance Company
Bending the Diabetes Cost Trend
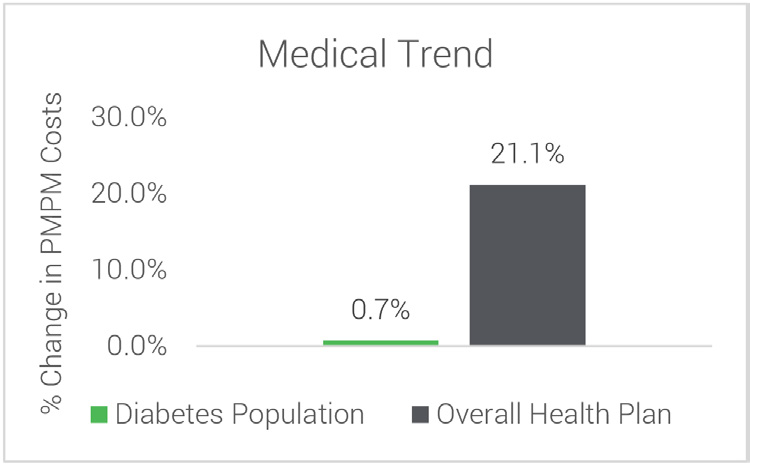
 A national insurance company saw a 20% increase in year over year costs of their population with diabetes due to poor adherence to care standards and high hospitalizations. To bend their cost trend, they implemented the Diabetes Care Rewards Program.
A national insurance company saw a 20% increase in year over year costs of their population with diabetes due to poor adherence to care standards and high hospitalizations. To bend their cost trend, they implemented the Diabetes Care Rewards Program.
Implementing the Diabetes Care Rewards Program meant a shift in thinking to provide a benefit enrichment that was confidential for the member and comprehensive in scope to attack the high costs drivers.
In the past ten years, our client has seen dramatic results as demonstrated by a 47% rate of engagement among employees, spouses and dependents, which is 3 times the national average for disease management programs.
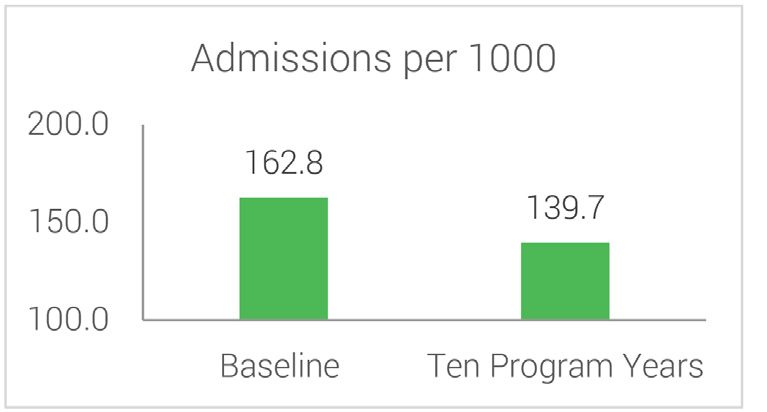
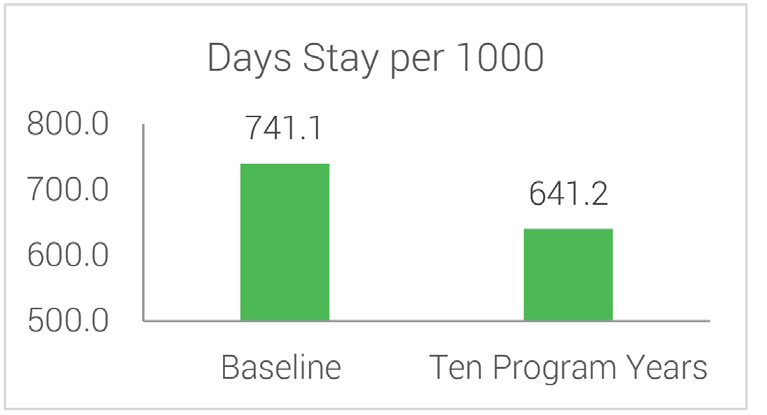
With increased adherence to care standards with members’ own doctors and improved medication adherence, the Program yielded significant reductions in both hospital admissions and length of stays for all members with diabetes.
Hospital Admissions & Days Stay Per 1000 Baseline vs 10 Program Years
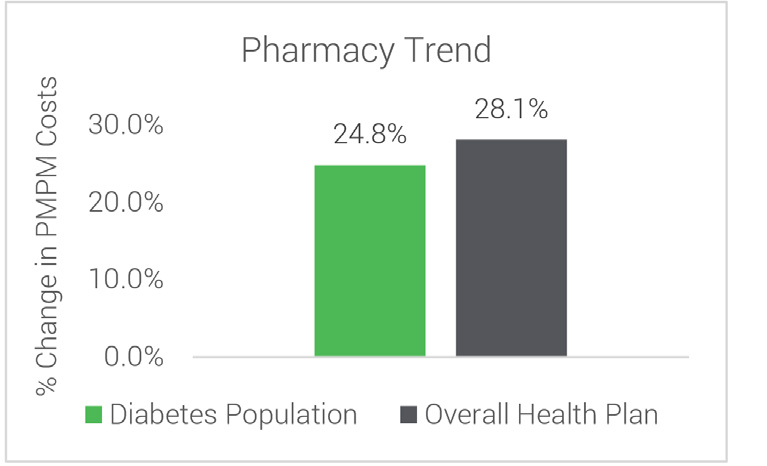
Cost Trends Over 10 Years Members with Diabetes vs Overall Employer Population
A1c Changes and Member Utilization
with an A1c >10
disease management programs
