Massachusetts Municipality
Bending the Diabetes Cost Trend
 Seeing rising medical claims driven by costly chronic conditions and a lack of member engagement with their care, a Massachusetts municipality, in an effort to bend their cost trend, implemented the Abacus Diabetes Care Rewards Program.
Seeing rising medical claims driven by costly chronic conditions and a lack of member engagement with their care, a Massachusetts municipality, in an effort to bend their cost trend, implemented the Abacus Diabetes Care Rewards Program.
Implementing the Program allowed them to provide a benefit enrichment that was confidential for the member and comprehensive in scope to attack the costs.
In the past seven years, the City has seen dramatic results demonstrated in terms of member participation, shifts in A1c and medical trend. Health plan members doubled the national average for participation among employees, spouses and dependents in disease management programs.
An A1c test is a key clinical measure for diabetes that shows blood glucose control over the past 90 days. The Program increased the number of members in more controlled ranges (A1c < 7) and dramatically reduced members not demonstrating glucose control (A1c > 9 & > 10), helping to reduce their risk for adverse events.
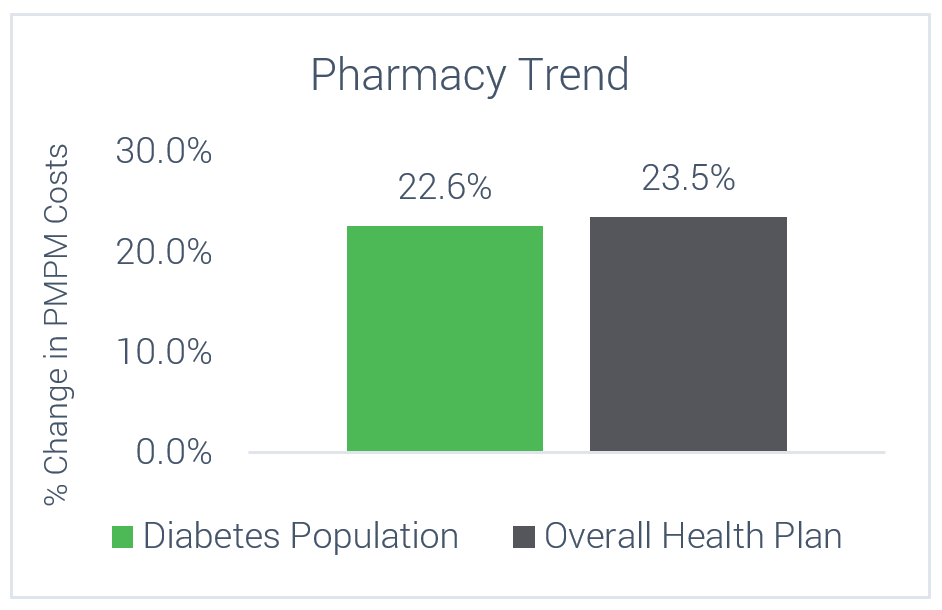
While using pharmacy-based incentives to support participants, the pharmacy costs for all members with diabetes was slightly less than the overall City’s pharmacy trend.
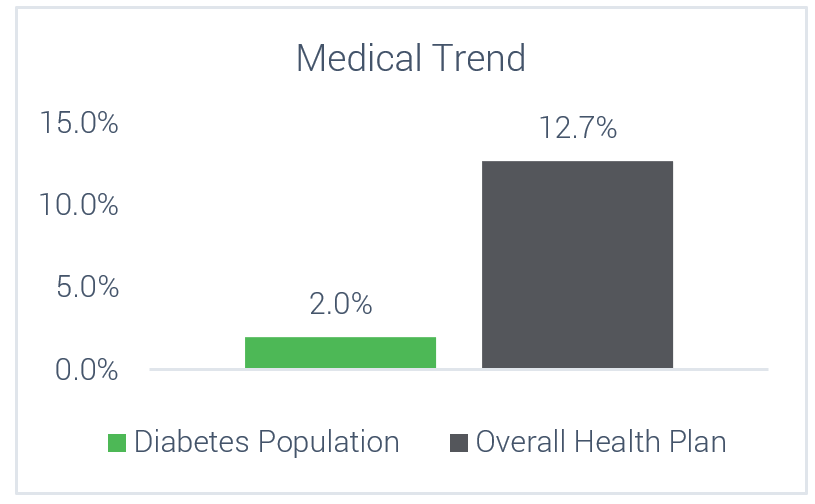
In addition to supporting the members on their diabetes journey, the Program was able to take diabetes from being a top cost driver for the City and reduce the medical claims trend well below the overall trend for the City. This saved the City millions of dollars in avoided healthcare costs.
A1C Changes and Participation Results
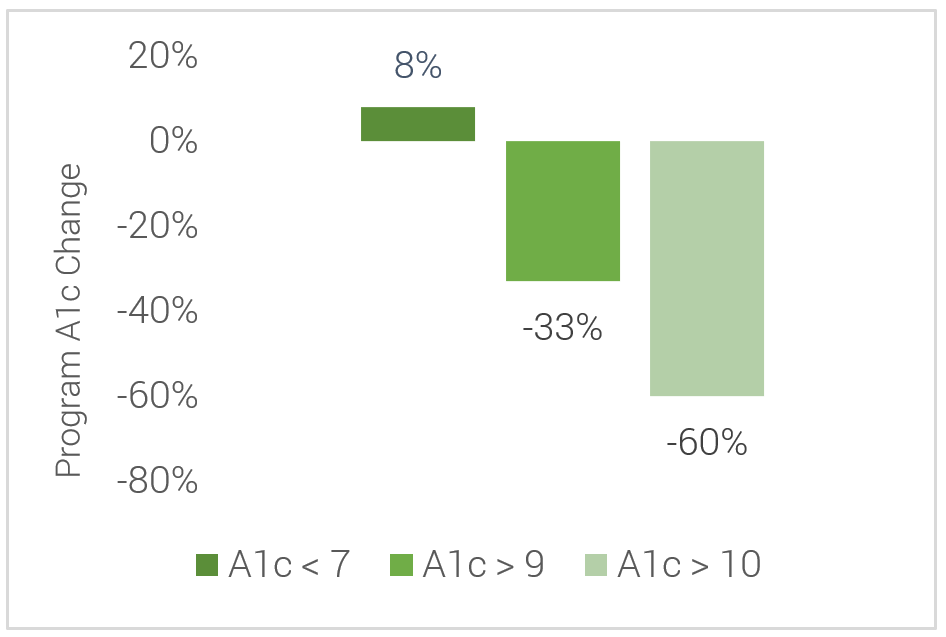
disease management programs
Cost Trends Over 7 Years
Members with Diabetes vs Overall Employer Population