Abacus Health Solutions (Abacus), a pioneer in behaviorally focused chronic health condition management, announces the publishing of Behavior-Based Diabetes Management: Impact on Care, Hospitalizations, and Costs in the American Journal of Managed Care’s March 2021 edition.
The study examines the impact of the Abacus’s Diabetes Care Rewards Program, a behavioral science approach and incentive based care management program on care, hospitalizations, and costs for a diabetes population. The program utilizes core principles of behavioral science and contingent incentives to drive completion of core diabetes care standards per the American Diabetes Association. Members who adhere to program requirements are rewarded using a patented copayment waiver process for all diabetes medications and supplies.
The study used retrospective observational cohort make up to compare utilization and cost data between individuals who enrolled in the Program and individuals who were eligible but not enroll. Nearly 14,000 individuals from 26 self-insured employers composed the pool of enroll and unenroll study participants. Members needed to have 24 months of continuous medical and pharmacy claims data within the Abacus data set. Members were then matched using a propensity scoring technique between 2010 and 2017, resulting in total study cohort of 3,318 with 1,659 in the enrolled and 1,659 unenroll.
On patient activation measures, the enrolled group showed better adherence to diabetes related care metrics like a 32% greater adherence to semi-annual HbA1c testing, along with a 20.1% decrease in members with an HbA1c >9. Enrolled members had an 80% greater likelihood to continue with their medication regimen.
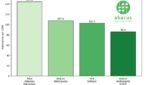
On utilization and cost measures, enrolled members had 38% lower all cause hospital admissions and 34% fewer days day, which drove a 21% lower medical trend for the enroll vs unenrolled population.
“The study provides a business case for employers and health plans to promote patient engagement though the use of relevant and behavior contingent incentives which lead to better health outcomes, reduced hospitalizations and lower costs.” said Michael Follick Ph.D. Abacus CEO & Co-Founder.